Bowel Cancer Screening
Bowel cancer screening can save lives. Screening aims to detect bowel cancer at an early stage, when treatment has the best chance of working. It’s available to everyone aged 60 to 74 years.
The test can also find polyps (abnormal clumps of cells which are non-cancerous growths in the bowel), which might develop into cancer over time. Polyps can be easily removed to lower the risk of bowel cancer developing.
Regular bowel cancer screening reduces the risk of dying from bowel cancer.
What is bowel cancer screening?
Each of the bowel cancer screening programmes in the UK use home tests called the Faecal Immunochemical Test (FIT). FIT looks for hidden blood in poo. If you’re registered with a GP and are within the eligible screening age range, a test will automatically be posted to you, so you can complete it in the privacy of your own home.
Since April 2021, through a 4 year phased approach, NHS England have gradually been reducing the age range for bowel screening to include people aged 50 – 59.
You will be invited to take part in screening every 2 years until you reach the age of 75. If you are over 75, you can ask for a kit every 2 years by calling the free helpline on 0800 707 6060.
If you are below the screening age and are worried you may have symptoms of bowel cancer, you should make an appointment to see your GP. Bowel cancer is more common in people over the age of 50, but it can affect anyone of any age.
You may be asked to take part in a research project (a ‘clinical trial’). Research helps the NHS improve Bowel cancer prevention and treatment for people in the future. You can choose whether to take part or not. Your choice will not affect your bowel cancer screening.
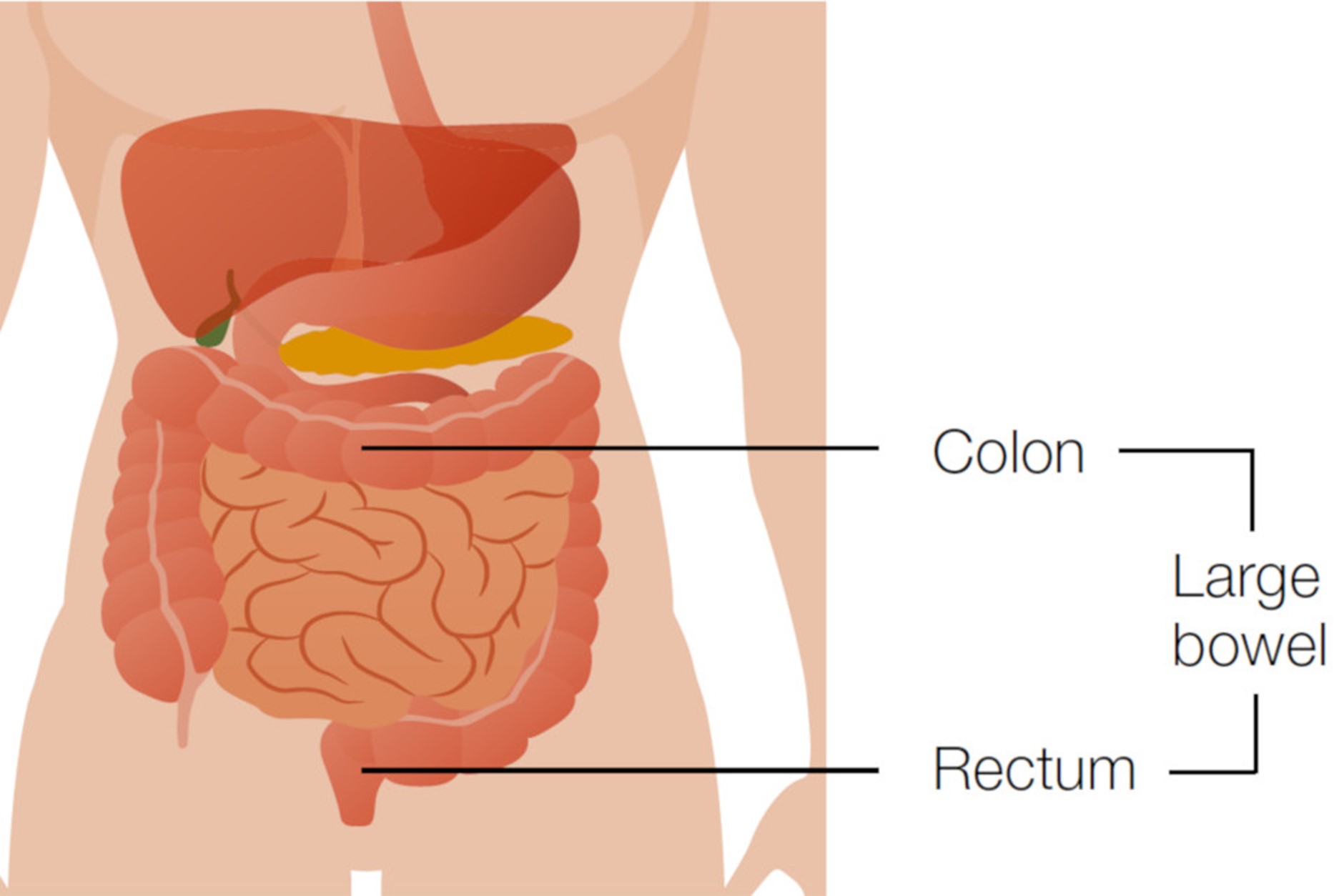
How the bowel works
The bowel is part of your digestive system. It takes nutrients and water from food and turns what is left into poo (also known as faeces, stools or bowel motions). As illustrated below, the colon and rectum make up the large bowel.
Bowel cancer
Bowel cancer is also known as colon, rectal or colorectal cancer. Sometimes the cells that make up the bowel grow too quickly and form a clump of cells known as a bowel polyp (some types of polyp are called an ‘adenoma’. Polyps are not bowel cancers but they can sometimes change into a cancer over a number of years.
Risks of developing bowel cancer
Everyone, whatever your sex, is at risk of developing bowel cancer. Things that can increase your risk include:
- Getting older (8 out of 10 people diagnosed with bowel cancer are over 60)
- Not being active enough
- Being overweight
- A diet high in red and processed meat and low in fibre, vegetables and fruits
- Smoking
- Drinking too much alcohol
- Having type 2 diabetes
- Having inflammatory bowel disease (ulcerative colitis or Chron’s disease)
- A family history of bowel cancer
Reduce your risk of developing bowel cancer
Having bowel cancer screening reduces your risk of dying from bowel cancer by at least 25%.
You can also reduce your risk of bowel cancer by:
- Keeping physically active
- Keeping a healthy weight
- Eating plenty of fibre – for example, choose wholegrain and wholemeal foods
- Eating plenty of fruit and vegetables
- Eating less red meat and especially less processed meat
- Drinking less alcohol
- Not smoking
How bowel cancer screening works
You will receive an invitation letter with information about bowel cancer screening. The information is to help you decide whether to take part. You will then receive a faecal immunochemical test (FIT) through the post.
Faecal Immunochemical Test (FIT)
The FIT test detects blood in your poo (blood you wouldn’t notice by eye). The reason we look for blood is because sometimes polyps and bowel cancers sometimes bleed.
The test consists of a small plastic bottle with a stick attached to the inside of the lid. This is used to take one small poo sample and then placed back into the plastic bottle and seal.
You will then need to put the sample into the self-sealing, freepost envelope and send it back to the laboratory for processing. Full instructions and a detailed information leaflet will be sent to you with your invitation and test. Using the kit takes just a few minutes and it’s an easy and effective way to screen for early signs of bowel cancer.
If you’re not sure whether you should use the kit, you can call a free helpline on 0800 707 6060 for advice. For example, if you have had surgery and have an artificial opening that allows poo from the bowel to pass (a stoma) then you may wish to call the helpline for further advice.
If the test finds anything unusual, you might be asked to go to the hospital to have further tests to confirm or rule out cancer. Finding blood does not diagnose bowel cancer, but, it does mean you need further tests (usually a bowel examination).
What happens to samples after testing
Once your FIT sample has been analysed, the results are recorded onto a database and the kit and its contents are then destroyed. The database information is kept to ensure you are treated correctly. It is also used to monitor the performance of the bowel cancer screening programme.
Bowel cancer screening results
You should receive a results letter within 2 weeks of sending in your sample and there will be one of 2 possible outcomes.
No further tests needed at this time
Most people (about 98 out of 100) have this result. It means there wasn’t any blood found in your sample, or only a tiny amount which is within the screening range.
This result does not guarantee that you do not have bowel cancer, or that it will never develop in the future.
Being aware of the symptoms of bowel cancer is very important. You will be offered bowel cancer screening again in 2 years time if you are under the age of 75.
Further tests needed
About 2 in every 100 people tested have this result. It means that an amount of blood was found in your sample which sits above the screening range.
This does not mean you have cancer, but it does mean you will be offered an appointment to discuss having a colonoscopy which usually takes place in a hospital. Colonoscopy looks at the inside of your bowel and are used to find the source of the blood.
There are several things that can cause blood in poo, such as:
- Haemorrhoids
- Bowel polyps
- Bowel cancer
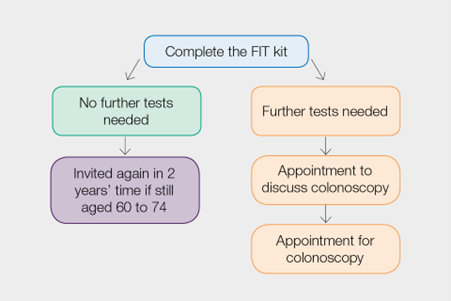 A specialist screening practitioner (SSP) will discuss your screening result with you and answer any questions you may have. They will discuss the colonoscopy with you in more detail and check to make sure you are fit enough for the procedure.
A specialist screening practitioner (SSP) will discuss your screening result with you and answer any questions you may have. They will discuss the colonoscopy with you in more detail and check to make sure you are fit enough for the procedure.
If you are fit enough for a colonoscopy and wish to proceed with the examination, an appointment will be arranged for you. If the SSP does not think you are fit enough for the procedure, you may be offered an alternative investigation such as a computerised tomography (CT) scan (sometimes referred to as a ‘virtual colonoscopy’).
Colonoscopy
Colonoscopy looks at the lining of your large bowel. A colonoscopy specialist passes a thin flexible tube with a tiny camera attached (a colonoscope) into your back passage (rectum). They guide the colonoscope around your large bowel. If they find any polyps, they can usually remove them painlessly using a wire loop passed down the colonoscopy tube. They will check any removed polyps for cancer cells.
Colonoscopy is the best way to diagnose bowel cancer. For most people, colonoscopy is straightforward. But as with most medical procedures, complications can happen. These can include:
- A hole (perforation) in the bowel caused by to colonoscope (around 1 person in 1,700); around half of people with a perforation will need surgery to repair it
- Heavy bleeding needing a transfusion (around 1 person in 2,400)
In very rare cases, people have died following colonoscopy complications. However, the most recent published national colonoscopy audit recorded no deaths. The audit looked at 20,085 colonoscopies carried out for both screening and symptom investigations.
For more information, you can read the leaflet about colonoscopy.
Possible benefits and risks of bowel cancer screening
Being aware of the possible benefits and risks will help you decide whether or not to take part in bowel cancer screening.
Benefits:
- Reduces your risk of dying from bowel cancer by at least 25%
- Allows for removal of any polyps found during colonoscopy, which reduces the risk of developing bowel cancer
- Can be completed at home in private
Risks:
- Cause complications, for example during or after colonoscopy
- Miss a cancer if it was not bleeding when you use the FIT kit
- A polyp or cancer can sometimes be missed if it was not bleeding when the screening test was taken (a ‘false negative’ result)
- Bowel cancer may develop in between screening tests
It is important to be aware of the symptoms of bowel cancer even if you have screening. No screening test is 100% effective. If you do not need further tests after using the FIT kit, this does not guarantee that you do not have bowel cancer, or that it will never develop in the future.
Bowel Cancer symptoms
Symptoms of bowel cancer include:
- Blood in your poo (faeces)
- Looser poo, pooing more often and/or constipation
- A pain or lump in your abdomen (tummy)
- Feeling more tired than usual for some time
- Losing weight for no obvious reason
Always see your GP if you have symptoms of bowel cancer at any age, even if you have recently completed an NHS bowl cancer screening test kit – do not wait to have a screening test.
Treatment for bowel cancer
A diagnosis of bowel cancer is unlikely. But, if it does happen, you will be referred to a team of specialists who will look after you.
If the cancer is a polyp removed during a colonoscopy, regular check-ups may be all you need.
The main treatment for bowel cancer is surgery. In some cases, the specialists may offer you chemotherapy or radiotherapy.
Not all bowel cancers found at screening are curable. But for people who have bowel cancer found at its earliest stage, over 90% are still alive 5 years later.